Noonan syndrome
Codes
ICD-10: Q87.1E
ORPHA: 648
General information
Estimated occurrence
40-100:100,000 live births.Cause
Autosomal dominant hereditary trait. The mutation is known in 75 % of cases.General symptoms
Most children born with Noonan syndrome have some kind of cardiac defect. Short stature – adult individuals with Noonan syndrome are generally about 15 cm shorter than predicted height. Growth hormone production deficit. Late onset puberty is common, and in many boys the testicles remain undescended. Some individuals have delayed psycho-motor development and intellectual disabilities. There may be some increased tendency to bleed, but this is not severe.Images
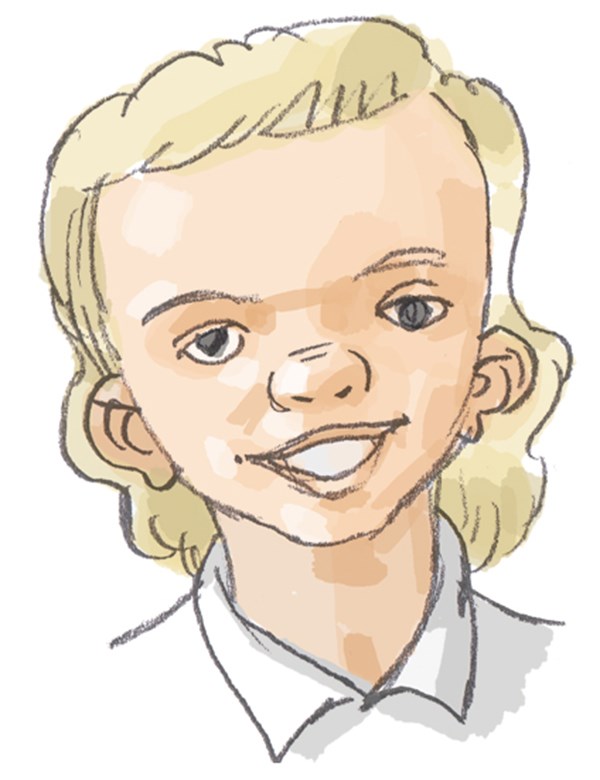
Characteristic facial features in Noonan syndrome:
Broad forehead. Short and broad neck. Low hairline at the nape of the neck. Low-set ears. Backward rotated ears. Drooping eyelids (ptosis). Almond-shaped eyes. Eyes slant downwards. Widely set eyes (hypertelorism). Skin fold (epicanthal fold) in the inner corner of the eye.

Orofacial/odontological symptoms
Characteristic facial features are associated with the diagnosis. Feeding difficulties are common, particularly during the first years of life. Some children have a great deal of vomiting. Owing to eating and swallowing difficulties, some children with Noonan syndrome need to eat often, and require a special diet. This may lead to an increased risk of tooth decay. High palate, late teething and small jaws with closely-spaced teeth have all been reported.Advice on follow-up and treatment
- Children with eating disorders often require extra dental care, including assistance with oral hygiene and fluoride treatments. However, the dental services should not advise on eating difficulties.
- Regular check-ups of dental and jaw development. Orthodontist should be consulted when needed.
- An increased tendency to bleed may result in complications when teeth are extracted.
- Oral motor training and stimulation may be relevant in cases of eating difficulties, speech impairment and drooling.
- Feeding and swallowing difficulties are investigated and treated by a specialist team at the hospital or multidisciplinary treatment center.
- When treating medically compromised patients always contact their doctors for medical advice (bleeding problems, heart diseases etc).
Sources
National Board of Health and WelfareUpdated: 2019-11-12 15:03






