Duchenne Muscular Dystrophy
This is the text from the oral care programme for people with Duchenne muscular dystrophy (DMD)
Mun-H-Center, a Swedish orofacial resource center for rare diseases and a specialist dental clinic, has gathered knowledge and experience over many years regarding the clinical care of patients with Duchenne Muscular Dystrophy (DMD). This document compiles the most important experiences related to the treatment and care of this group of patients.
Background
Duchenne Muscular Dystrophy is a neuromuscular disease caused by a lack of dystrophin, which stabilises muscle fibres. The absence of dystrophin leads to a breakdown of the muscle fibers. Muscles are replaced by connective tissue and fat. The disease is inherited through the X chromosome. Women who carry the gene have no symptoms. In about one-third of all cases, the disease occurs through new mutations.
Symptoms usually appear around the age of three. The child develops a difficulty running, jumping and getting up from the floor. Generally, boys stop walking between 10 and 12 years of age. Over time, muscle weakness increases. Respiratory muscles weaken and lung function deteriorates. Heart function may also be affected. Weakness occurs in the large chewing muscles, facial muscles and tongue. Bite abnormalities develop progressively due to muscle weakness and changes in tongue morphology. The jaws increase in width, more in the lower jaw than the upper, leading to crossbite. It is common for the bite to open in the side sections and later in the front teeth area. The ability to open the mouth may be restricted.
Sensitivity to malignant hyperthermia has been reported and should be considered during anaesthesia. Concentration difficulties and developmental disorders may occur. Extensive research is ongoing to lessen and slow down symptoms.
Dental care for people with DMD
Need for preventive dental care
It is important for children to establish early contact with dental care, preferably with a paediatric dentist. Individuals with DMD require regular and enhanced dental care to maintain good oral health. It is important to record the ability to open the mouth during annual dental check-ups. If there is a decrease in the ability to open the mouth, jaw joint function should be investigated and appropriate treatment initiated.
Risk factors for oral health
A reduced ability to open the mouth can make it difficult to perform oral and dental care. Due to this, it is important to plan ahead for potential extractions of molars including wisdom teeth. If oral motor function is affected, one should be aware that food may remain in the oral cavity after meals, increasing the risk of caries and periodontitis. Inactive oral motor function often leads to increased calculus formation. Reflux and nausea can cause erosion damage to the teeth. In later stages of the disease, many require respiratory support. Respiratory support combined with an open mouth at rest increases the risk of dry mouth.
Guidance for relatives, assistants and caregivers
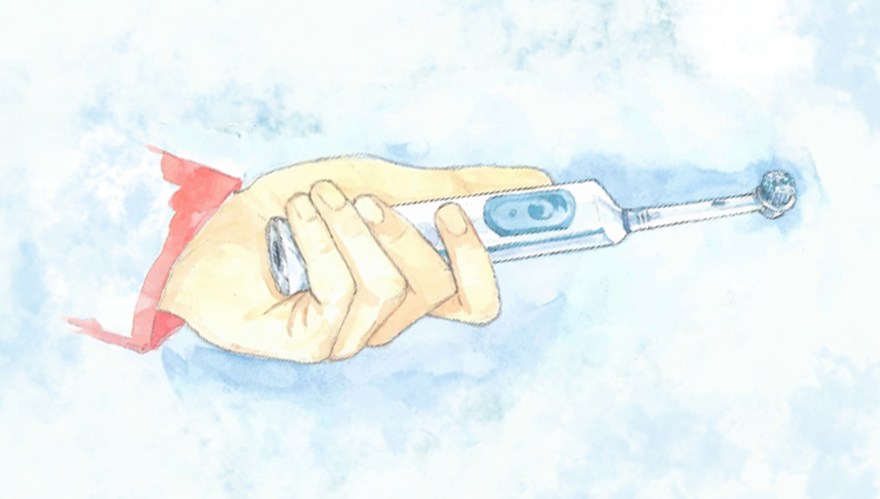
People with DMD may need help with their oral care at home. To do this in the best possible way, they need practical guidance from dental care professionals and access to oral
care aids.
About the oral care programme
Authors: Anna Ödman Roussakis, specialist dentist in orthodontics, Annette Carlsson, dental hygienist, Lisa Bengtsson-Stelzer, speech language pathologist, and Åsa Mårtensson, hospital dentist, Mun-H-Center.
Layout and photos: Inga Svensson, previous communicator, Mun-H-Center.
Illustrations in the exercise program: Komhit.
Translation: Hanna Samara, communicator, Mun-H-Center.
Cover image: Eva Kraft.
Print: 2024









