Myotonic dystrophy type 1
Codes
ICD-10: G71.1
ORPHA: 273
General information
Estimated occurrence
12:100,000 inhabitants.Cause
DM1 is a neuromuscular disease with autosomal dominant heredity. DM1 is caused by a defect (tricucleotide expansion) on the DMPK gene on chromosome 19 (19q13.3).General symptoms
There are four sub-groups of DM1 depending on age at onset: congenital, childhood, classical and mild. In general, the earlier the symptoms occur, the more severe the clinical symptoms of the disease will be. DM1 is a neuromuscular disease with muscle weakness, muscle wasting and myotonia (delayed muscle relaxation) as cardinal symptoms. Multiple systems can be affected such as the heart, smooth muscle, brain, endocrine regulation and skin. Most individuals with congenital and childhood DM1 have learning disability and the frequency of neuropsychiatric disorders is higher than in the general population. The disease has a slowly progressive course.Synonyms
Steinert's muscular dystrophy.
Images
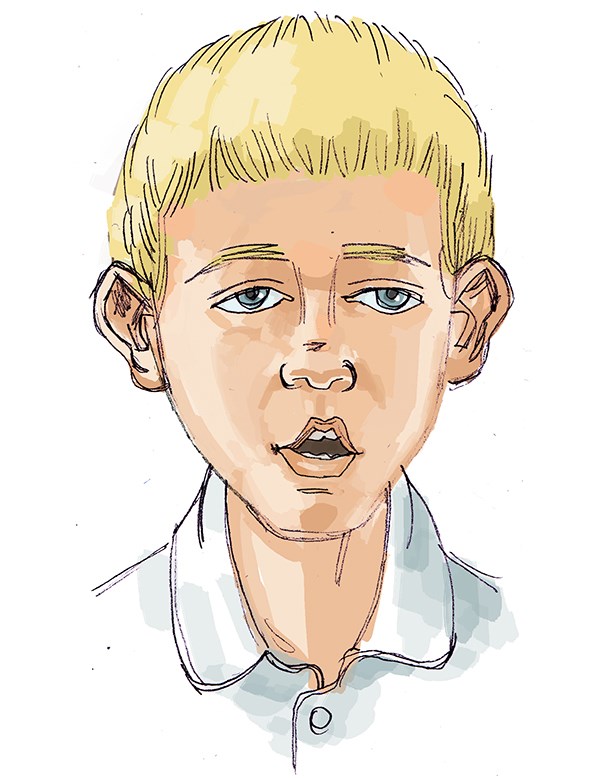
Characteristic facial features in myotonic dystrophy type 1:
Impaired facial expression. Longface. Hanging eyelids. Open lips. Triangular shaped mouth. Open bite.

Orofacial/odontological symptoms
Sucking difficulties and breathing problems are common in newborns. Weak orofacial muscles may lead to impaired facial expression, open mouth posture and difficulties with eating, speech and saliva control. The muscular wasting may affect facial growth and cause malocclusion. Some have problems with the temporomandibular joints and impaired jaw opening capacity. There is also an increased risk for caries and gingivitis in individuals with dry mouth and impaired self oral clearance. An increased sensitivity for general anaesthesia drugs has been reported.Advice on follow-up and treatment
- Early contact with dental services for intensified prophylactic care and oral hygiene information is essential.
- Regular check-ups of dental and jaw development. Orthodontist should be consulted when needed.
- In cases of temporomandibular joints disorders, this should be investigated and appropriate treatment thereafter prescribed.
- Orofacial therapy and oral motor skills training in cases of difficulties with eating, speech or drooling.
- Speech, language and communication training are often required.
- When treating medically compromised patients always contact their doctors for medical advice.
Sources
National Board of Health and WelfareUpdated: 2019-11-12 14:36






